The Future of Autism Care Starts at Home
Shorter sessions. Stronger outcomes. A model built for families — not billing.
Bullets to sound smart with your friends (or your boss):
ABA grew to ~$5B by treating therapy as billable time, not an optimal outcome. Huey flips the script with short, virtual coaching sessions led by parents—not 20–30 hrs/week in clinic.
Built for engagement: Huey meets families at key stress points—post-diagnosis, entering school, or adolescence—driving adherence and long-term use.
Power of parent-led care: Within six months, most Huey families hit clinical goals like improved compliance and fewer meltdowns—without overloading parents.
Better outcomes, lower costs: Over 80% of children reach goals using ~1‑2 hrs/week of coaching. Less burnout, lower spend per result—and families report higher confidence.
How ABA Therapy Took Over Autism Care
A $5B industry built for scale
A child is flagged for signs of autism. The family waits four months for an evaluation. When therapy finally begins, the behavioral tech quits. The next one is late, so progress stalls. The bill hits five figures. Insurance covers only part of it.
At home, parents are juggling IEPs, sprinting between jobs, and calming a sibling who doesn’t understand why their brother gets all the attention.
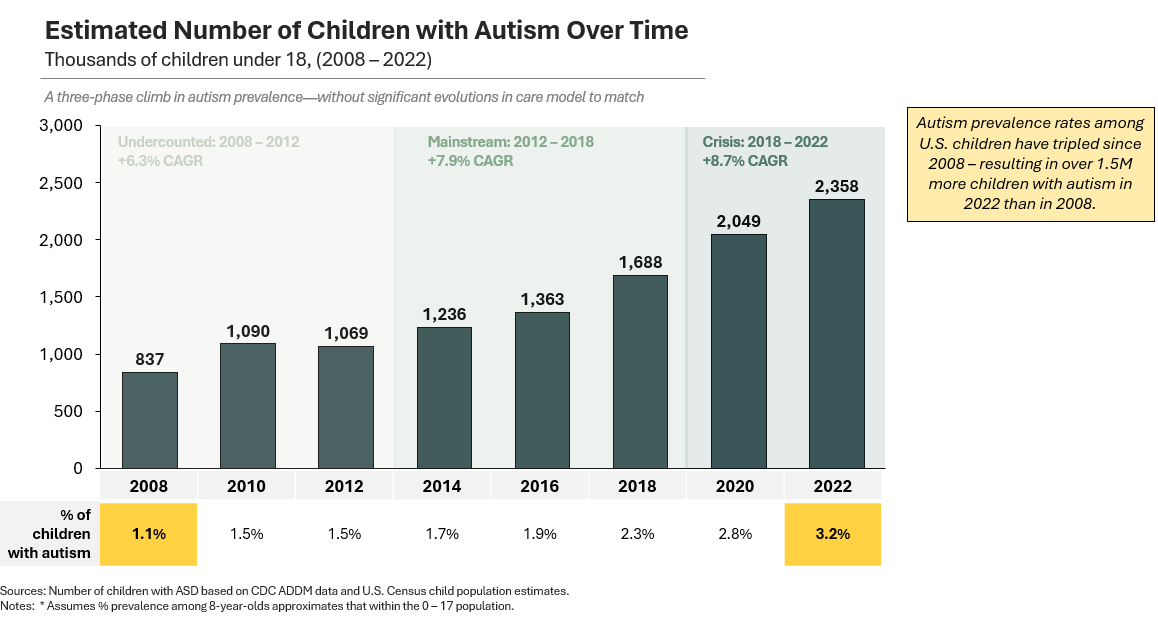
Each year, over 100,000 families begin this journey. More than 2.4 million children in the U.S. have an autism diagnosis. And that number keeps rising.
For the last decade, autism services have been dominated by a single model: Applied Behavioral Analysis (ABA). Delivered in-clinic and billed by the hour, ABA grew into a $5B+ industry with the support of private equity, who under-wrote its recurring revenue and rapid patient growth (BACB).
But that model’s tailwinds are fading:
The workforce is breaking: Turnover has peaked: 65% attrition for RBTs and 30% for BCBAs.
Gross margins are contracting: Though Medicaid rates have risen, they haven’t kept pace with demand. Job postings for RBTs and BCBAs are up 131% and 58% respectively (BACB).
Payers* are pushing back: At $90 / hour, 20 hours of weekly therapy adds up to ~$90K per year. With inconsistent access and limited outcomes data (even from groups like the NIH) that cost is hard to justify.
Note: * ABA is a pediatric service, so payers haven’t cut it outright. But in the past two years, cost containment has escalated: shorter prior-auth cycles, visit caps, and fee schedule freezes in states with previously elevated rates. United has tightened reauthorization requirements, and Q1 2025 earnings from Centene and Elevance cite rising Medicaid MLRs and heavier utilization management in outpatient care—though few name ABA explicitly.
Right as patient demand reached all-time highs in 2023, investor appetite cooled. Blackstone-backed CARD filed for bankruptcy. Elemy went through four rounds of layoffs before abandoning direct care.
This slowdown couldn’t come at a worse time. The CDC’s latest report estimates 3.2% of children have autism, 3x the prevalence reported two decades ago.
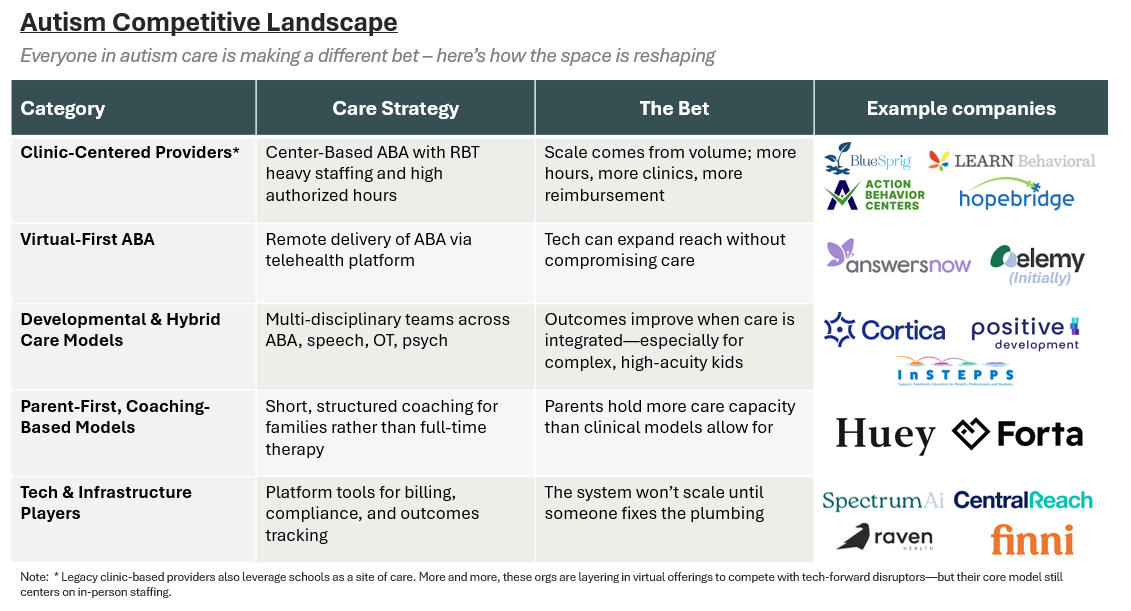
But as the old model buckles, investors are backing a new class of ABA provider—one betting on virtual delivery and parent-centered design as the more scalable, exit-ready path. (BH Business).
Huey Health is one of them. And it’s not alone. A new standard of care is emerging—less behavioral, more developmental—and built around families, not just therapists.
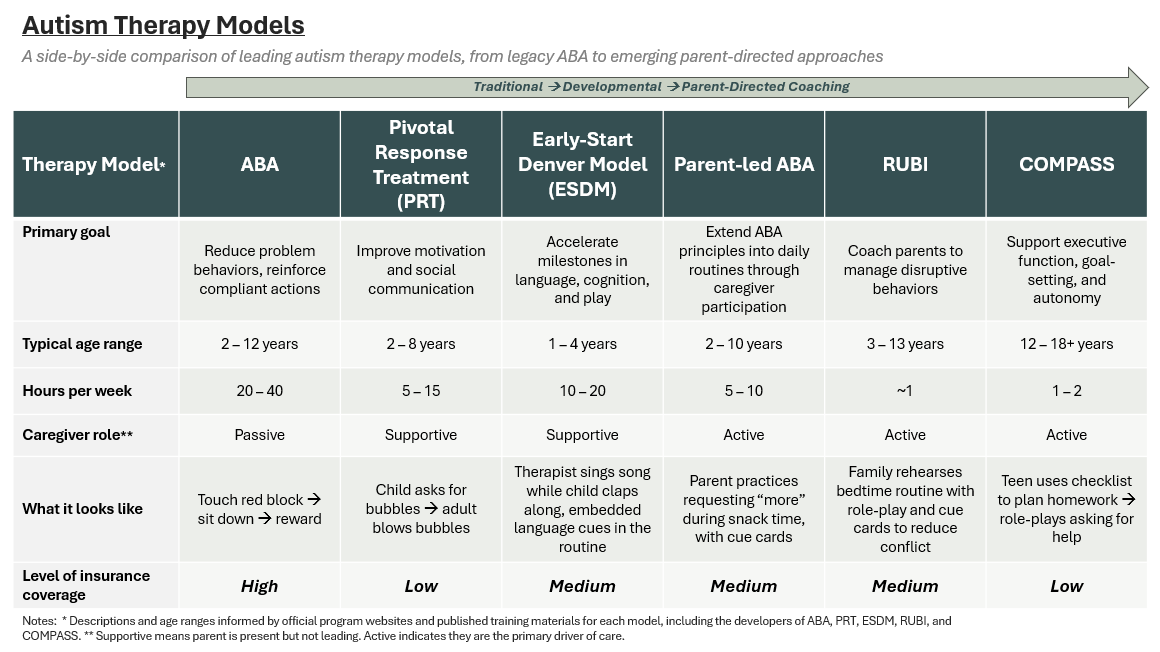
Here’s how some of these emerging clinical models compare:
Huey sits at the right end of that spectrum. Its core programs—RUBI, Compass, and Parent-Led ABA—reduce hours and cost. But more importantly, they deliver: Over 80% of Huey clients meet their clinical goals, as tracked by networks like Catalight.
We spoke with founder Raffay Mirza about the system Huey is rebuilding—and why he believes the future of autism care starts at home.
ABA was Built for Billing, Not Care
How CPT codes, staffing economics, and narrow licensure shaped the wrong system for families
For Raffay, the inefficiencies in autism care were personal. In Australia, where his father works as a disability planner, families are assigned a care coordinator after diagnosis to build a two-year care plan, which covers behavioral therapy, SLP, OT, family counseling, and feeding. Really, anything that’s needed.
“It’s holistic,” Raffay said. “Services are based on individual need, reimbursed through a national fee schedule. There’s no need to anchor care to a specific diagnosis to get paid.”
Then he moved to the U.S.
“Here, you’re handed a diagnosis, plus a list of in-network providers if you’re lucky,” he said. “The system centers insurance coverage, not the child’s needs.”
ABA’s meteoric rise was fueled by a wave of state-level insurance mandates, beginning in the late 90s and culminating in coverage requirements across all 50 states by 2019 (Autism Speaks). “Families come in asking for ABA after reading about it online,” Raffay said. “But what might help more is speech or executive function support. Not 30 hours of in-clinic therapy.”
Leading with CPT codes has structural implications for labor. For example, in California the Business & Professions Code restricts BCBAs to working only with children with autism, and only on narrow interventions. Clinicians are locked into code-driven services.
“Parents often need coaching,” Raffay said. “But under current rules, the only professionals who can bill for that are LMFTs or LCSWs.”
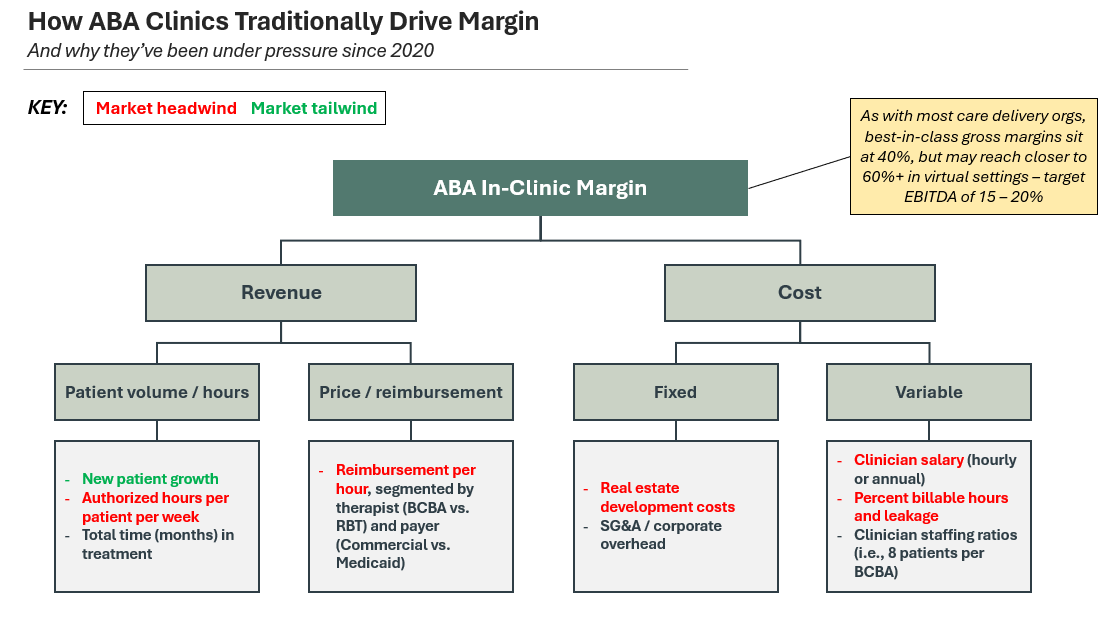
For providers, a billing-first world presents different challenges. “The reimbursement model doesn’t work unless you’re playing for volume,” Raffay said. “To get any leverage with payers, you need to offer network access. So, you’re scaling hours, or selling the business.”
For years, ABA operators relied on this fragile equation: long treatment arcs, high authorized hours, and predictable reimbursement. The model looked scalable, but it was predicated on razor-thin margins, high staffing ratios, and flawless execution.
With that balance falling apart, even well-run practices are stuck selling to the next roll-up.
But this is more than a money problem. It’s a fundamental challenge with the model. “ABA can be a helpful modality for high-acuity needs,” he added. “But it was never meant to carry the system on its own.”
The Case for Parent-Led Autism Care
A model that meets families at inflection points and builds around the one constant in a child’s life
For Huey, the leading edge begins at home.
“When families begin with an in-clinic RBT, the mindset is passive—services are being done to me,” founder Raffay Mirza said. “When we flip it, parents realize: I have a role to play. The mindset shift drives long-term adherence.”
In traditional ABA, parents often wait for professionals to ‘fix’ the child. Huey makes it clear from the start: you’re in the driver’s seat.
It’s intuitive. Parents already spend more time with the child than any provider ever could. Huey builds around that truth—with three structured programs:
RUBI, for parents of younger children with disruptive behaviors
COMPASS, for teens and young adults navigating executive function, routines, and independence
Parent-led ABA, for a small proportion of children with high-acuity needs
All are delivered via virtual coaching sessions, coupled with tools families can use between visits: visual schedules, role-play scripts, token boards, and individualized behavior plans.
Beyond structure, Huey leans into timing—showing up to meet families at key transitions—after diagnosis, during school entry, or when burgeoning adolescence surfaces new challenges.
“Those windows are critical,” Raffay said. “We urge our payers to help us reach families before the system grinds them down.”
That said, Huey’s model isn’t for every household. Success depends on having a consistent, engaged caregiver. Without that foundation, things fall apart.
“We serve Medicaid families every day,” Raffay said. “This isn’t concierge care. But it does require parental buy-in.”
“The goal here isn’t labor arbitrage,” he added. “It’s a bet that parents—when equipped properly—can do more than we’ve allowed them to.”
Other models have tried to formalize that instinct. Forta experimented with paying parents to deliver care. They’ve since pivoted, but that’s a different wager entirely.
“It hasn’t been well-received,” Raffay said. “You shouldn’t have to professionalize your love for your kid just to get help.”
Autism Care Built to Last
Better margins. Better outcomes. No burnout.
Huey’s model offers something rare in autism care: resiliency. Two of the most volatile inputs in autism care—clinic real estate and RBT labor—are all but neutralized.
Staffing seven hours of direct therapy per day is unheard of (no more 75% utilization targets). Hitting those numbers requires near-perfect staffing. One no-show, late hire, or RBT dropout can collapse the entire week’s margin.
Instead, Huey care teams spend a few focused hours coaching families and preparing custom materials. The unit of care isn’t the session. It’s the parent’s ability to keep things going after the session ends.
The result? Happier clinicians → better retention → better care → improved outcomes.
And the economics hold up; Huey’s margins look more like a SaaS company than a service provider.
On outcomes, light doesn’t mean loose. Goals are defined up front and tracked in collaboration with partners like Catalight, which approves every care plan and reviews outcomes across a range of family-reported and observational metrics.
“We don’t just track tantrum reduction or routine compliance,” Raffay said. “We measure how well the parent is implementing the strategy over time. That’s the intervention.”
This shift in the center of gravity—from provider to parent, from hours to agency—is more honest. Payers want value, and families want trust. This is where they meet.
The Future of Autism Care – If Huey’s Right
From high-hour to high-context. Built for the arc, not the episode.
Huey doesn’t treat autism as an episode of care. It isn’t trying to replace ABA either.
It’s trying to deliver what ABA was supposed to unlock: modular care that flexes with the family—starting with RUBI after diagnosis, shifting into COMPASS during adolescence, layering in higher-touch programs if needed. Families and payers step in when life changes; and step back when it doesn’t.
Consider LaRo—a young boy who had already spent three years in traditional ABA. His family came to Huey with no practical strategies. Within six months of RUBI, they’d hit every clinical goal: fewer meltdowns, stronger compliance, and a parent confident enough to carry the work forward without constant supervision.
And it matters—to families navigating jobs, tech gaps, and language barriers. To clinicians who want to stay in the field. To payers who want results without breakage.
If Huey scales as intended, autism care won’t revolve around authorizations or leases.
It’ll revolve around the people already doing the work.
That’s not just more human. It’s how care should have worked all along.
Not sponsored—just a model that deserves attention. If you’re building, investing, or operating in this space, you can reach Raffay at raffay@joinhuey.com.
Bonus: The New Autism Care Landscape
Huey is part of a broader shift that rethinks not only who delivers care, but how it’s designed, reimbursed, and scaled. Here’s how that landscape is taking shape:
💭 If this sparked something—hit the 💜 or leave a comment. I’d love to know what’s worth unpacking next. Or forward it to someone building in the space.
Liked this one? You might also like The Ambient Scribe Stack — a breakdown on how companies like Abridge, Ambience, and DAX are going beyond the note to rewire clinical workflows.
In-Network is where I write about the business of care: models, margins, and the infrastructure behind how we deliver it.
→ Subscribe for sharp, honest analysis on what’s actually changing in healthcare.



Great article. Until recently, many children in NZ are not spotted as having autism and have slipped though the net, not realizing there is a problem until young adulthood (well the ones I'm related to anyway). I'm going to share this with a friend of mine that works in this area.
After spending almost 15 years doing parent-led therapy in home, my wife and I launched a parent-led app (happyladders.com) launched two years ago to address this exact issue.
We’re seeing the same results as Huey. Parents are spending about 42 minutes per week and their child gains an average of of 24+ developmental skills.
This is the way. Great to see others pushing the ball forward! Such a great option for so many families.