What WISeR Gets Right About Medicare Reform
A small model with big implications. Less theory, more control.
WISeR in four bullets (for your boss, your deck, or your next 1:1):
320+ people were charged in a $14.6B federal healthcare fraud case; WISeR aims to block that kind of abuse before claims are paid
WISeR is one example of CMMI prioritizing execution over ideology — proof that not every model needs to be a moonshot
Providers who opt in may get faster claims and gold card status; those who don’t still face review, just with less control
WISeR could quietly enforce site-neutral care by denying high-cost settings without touching the fee schedule
America’s largest healthcare fraud case just made headlines: 320+ people charged, $14.6B in attempted Medicare and Medicaid fraud.
In hindsight, the schemes weren’t exotic — they were obvious. One transnational group bought over 30 DME companies, stole identities from 1M seniors, and submitted fake claims; they collected nearly $1B in catheter and glucose monitor reimbursements before CMS caught on.
That’s the problem. The U.S. healthcare system is complex enough to confuse and fragmented enough to exploit. This isn’t just a fraud problem — waste alone drives up to 25% of healthcare spending today.
Enter WISeR: a prior auth demo that brings targeted, tech-enabled control to the parts of Medicare most vulnerable to abuse.
No convoluted financial scaffolding. Simplicity is the innovation.
What is WISeR?
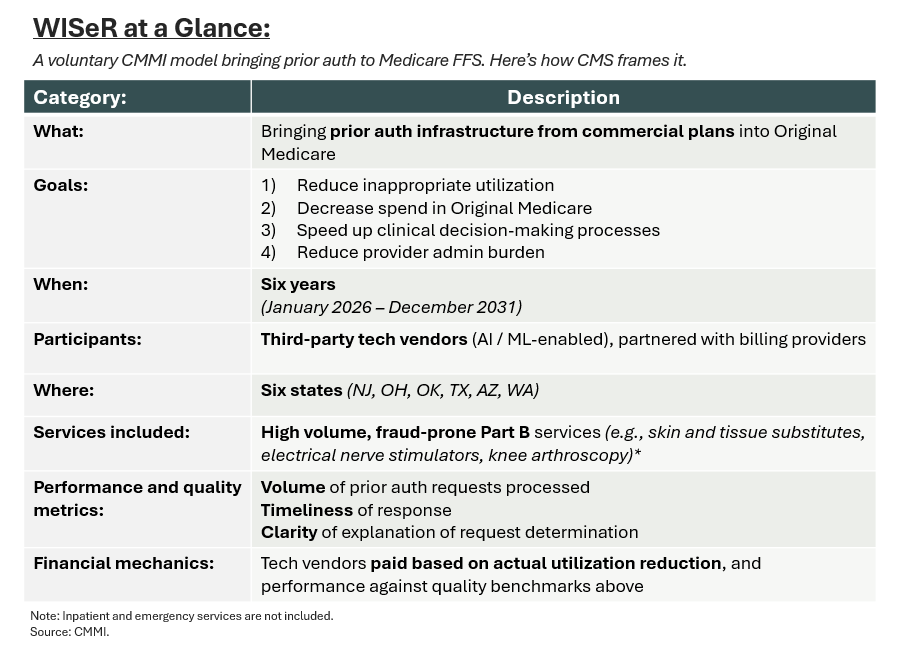
Launching in 2026, the “Wasteful and Inappropriate Service Reduction” (WISeR) model introduces prior authorization into fee-for-service Medicare. It does this not through MA plans, but directly via third-party technology vendors, who help determine whether or not a potentially harmful procedure (i.e., a knee arthroscopy) is clinically appropriate for someone age 65+. Here’s how CMS itself is framing it:
Why Would Anyone Join?
Participation in WISeR is voluntary. Without shared savings or risk upside (which fueled the proliferation of PE-backed ACOs), it’s fair to ask why anyone would bother.
My take: opting out doesn’t mean escaping scrutiny. Providers who sit on the sidelines will still face traditional medical reviews, but without the benefit of a structured pathway. Enrolling — and laying the groundwork alongside CMS-approved vendors — could mean faster claim processing and, eventually, gold-card status later down the road.
Engage early, shape the rules, and reduce uncertainty. Opting in might be the least risky move.
How This Differs from Other Innovation Models
Compared to prior CMMI demonstrations, WISeR’s structure is unusually clean. No attribution. No benchmarks. No downside risk.
This isn’t transformation theater — and that’s a feature, not a bug.
Let’s zoom out. Most CMMI models require a leap of faith. Programs like ACO REACH, CKCC, and TEAM show promise, but their success hinges on chained logic: if behavior changes → utilization drops → costs go down. Often, that bet is on care management.
I’ve backed companies that navigate this well (like Strive and Empassion). But still, they depend on proving savings through tight execution, and many don’t share their success. Discounted benchmarks can help, but they rarely bend the cost curve on their own.
WISeR is different. It’s a single-step intervention: control inappropriate utilization, reduce spend. The outcome is built into the mechanism — not dependent on provider behavior or attribution algorithms.
From the outside looking in, this is exactly what CMMI was built for: sharp, executable, and inflation-aware.
“The Secretary shall focus on models that the Secretary determines have the potential to reduce program costs … while preserving or enhancing the quality of care received by individuals.” – Section 1115A of Social Security Act (source)
There’s a broader context too. As AI-driven tools like ambient scribes improve documentation and coding, more claims will get paid — even ones that previously would’ve been rejected.
In 2024, an estimated $31.7B (7.66%) of Medicare FFS payments were improperly paid, either over or under the correct amount (source). WISeR may be CMS’s quiet acknowledgement that inflationary pressure is no longer downstream. It’s embedded in how care is coded, approved, and paid.
The Future of Medicare Reform
Outside of the three services mentioned, it’s still unclear which CPT or HCPCS codes WISeR will target.
But reading between the lines, categories like DME, labs, imaging, and other “low value” Part B procedures look like obvious candidates.
Just a theory, but in the future, this may be about more than utilization.
CMS has already experimented with site-neutral payment through the Outpatient Prospective Payment System (OPPS), aligning reimbursement between HOPD and physician offices. This was done first for E&M visits, but expanded to certain imaging, diagnostics, and minor procedures.
But admittedly, the success here was nominal — riddled with carve outs and undercut by grandfathered HOPDs billing at higher rates.
After some proof points, WISeR could build on that philosophy. Not by impacting rates, but by denying high-cost sites when lower-cost settings are clinically appropriate.
Think site-neutral payment — without touching the fee schedule.
That might scare some folks — and to be clear, I’m not saying this is good or bad policy.
But it’s worth naming as a structural mechanism to influence site-of-service decisions.

If that’s where this is headed, WISeR may influence the fundamentals of care: site, service, sequence.
And that’s what Medicare reform should look like: less ideology, more infrastructure.
💭 If this sparked something — hit the 💜 or leave a comment. I’d love to know what’s worth unpacking next. Or forward it to someone building in the space.
Liked this one? You might also like The Ambient Scribe Stack — a breakdown on how companies like Abridge, Ambience, and DAX are going beyond the note to rewire clinical workflows. Or After the GLP-1 Gold Rush, our take on what comes next for compounders and payers in the weight loss era.
In-Network is where I write about the business of care: models, margins, and the infrastructure behind how we deliver it.
→ Subscribe for sharp, honest analysis on what’s actually changing in healthcare.


