Modular AI, Trust, and Saying No with Camber's Nathan Lee
Beyond note-taking, how to build modular infrastructure for the clinics that got left behind — one clean block at a time.
This is a new format we’re testing: fast, founder-forward interviews from the front lines.
If you work in health tech, you've probably heard Camber’s name in a few sharp circles (fka Juniper), or seen their modular RCM stack in unexpected places. With Tier 1 VCs behind them, here’s what they’re building, and why it matters.
Why I Believe in Camber:
Build for the clinics that need it most. Fragmentation isn’t a flaw — it’s the foundation. Camber leans into speed, trust, and durability in places others ignore.
RCM isn’t back-office, it’s game theory. Camber plays offense: forecast deposits, surface risk, and fix problems before they hit the books.
Most AI moves fast, even when we’re not sure where it’s going.
Camber starts by cleaning the inputs, so we can see what care is actually delivered, what gets paid, and where value gets lost.Growth is easy, saying no is hard. Camber grows by staying clean, modular, and trusted — even when everything’s pulling it to expand faster.
Why RCM?
Revenue cycle (RCM) isn’t glamorous, but it’s the plumbing that makes everything else possible. In the U.S., even basic billing means navigating payer rules, modifier codes, and denial appeals. Small practices struggle to stay afloat, let alone grow.
While health systems have invested millions into EHR integrations and automated workflows, the mom-and-pop clinics that power Medicaid, primary care, and behavioral health are being left behind.
I’ve seen firsthand how broken RCM can drag down even well-resourced health systems. But for these clinics, this isn’t a matter of efficiency. It’s survival.
Independent practices drive access in rural and low-income markets, but they’re buried in admin drag, without the dollars or headcount larger orgs rely on.
Most vendors treat them as unscalable. Camber treats them as the starting point. They need tools that are modular, fast to deploy, and trustworthy out of the box.
They’re building an AI-first platform to automate and optimize revenue cycle for independent outpatient clinics — led by engineers and operators who know the space. Think: prior auth, eligibility checks, billing codes, and claim status — handled automatically.
Camber’s bet: that the next layer of healthcare infrastructure will be won by those who serve the messiest, most trust-sensitive parts of the system.
That’s why I sat down with Co-Founder Nathan Lee. He and the Camber team are building AI infrastructure for the long tail. We talked about provider fragmentation, trust as a wedge, and why the hardest decisions aren’t what to build, but when.
Q1: Many RCM startups are chasing large care delivery orgs. Why bet on small, independent specialty clinics instead?
Because they’re everywhere, and no one’s building for them. Fragmentation isn’t going away. In specialties like pediatric behavioral health (where we started), trust lives locally.
Independent clinics feel the most pain — and move fast to fix it. They’re led by clinician-owners: mission-driven, deeply committed to care, but not always set up to run a business. Maybe they broke off from a larger system. Maybe they’re treating a condition they’ve lived through themselves. Either way, BPOs and legacy systems aren’t serving their needs.
Hospitals are attractive — big dollars, rich data. But they’re slow. With small clinics, you can go from zero to running their whole stack in weeks. We found faster paths to data through mid-market enterprise deals.
And the tooling is different. Enterprise systems run on Epic or Athena. These clinics use specialized EMRs built on clinical need, but the RCM tools bundled with them are usually an afterthought. Our pitch is simple: we don’t touch your clinical. Let us fix your books—the part you shouldn’t have to think about.
Q2: If Camber wins, what unlocks for small clinics — not just financially, but culturally or structurally?
If we win, getting paid becomes a non-issue.
It’s like running a local coffee shop: you make someone a drink, they tap their card, and you get paid. That’s how care should feel. Automatic, not anxious.
When that stress disappears, two things unlock.
First, growth: you can take people off the waitlist, expand your team, maybe open new sites.
Second, confidence: you stop feeling like an underdog. You start thinking like an enterprise operator — because now you run like one.
That’s our worldview. Care should be personal. Infrastructure should be invisible. The plumbing should just work — and we’re here to make sure it does.
Q3: In these markets, trust is everything. What makes a clinic say: I’m willing to hand this over to you?
We earn trust by helping clinics move from playing defense to offense. RCM shouldn’t be retrospective; it should be prospective.
Most of the clinics we work with have been stuck with reactive BPOs. If deposits come in low, they’re staffed to chase down the issue. No visibility. No forecasting. Just stress.
Even a live-updating report showing where every dollar is sitting feels like a breakthrough. That transparency gives clinicians back control.
We can forecast what deposits should look like on any given day, and flag when something’s off. The same goes for claims: we don’t just report what got denied, we show what’s likely to get paid before it’s submitted.
That’s when trust develops. The tool helps you stay ahead.
Q4: RCM is where AI goes to die. How do you build flexible systems that hold up — and what’s one thing you had to build that surprised you?
Some startups use modularity to sell faster. We use it to stay disciplined — solving what’s real before chasing what scales.
Automation breaks when it’s built for a single, rigid workflow. Maybe it works for verifying benefits with a Blue Cross card. But as soon as it’s Aetna, it falls apart.
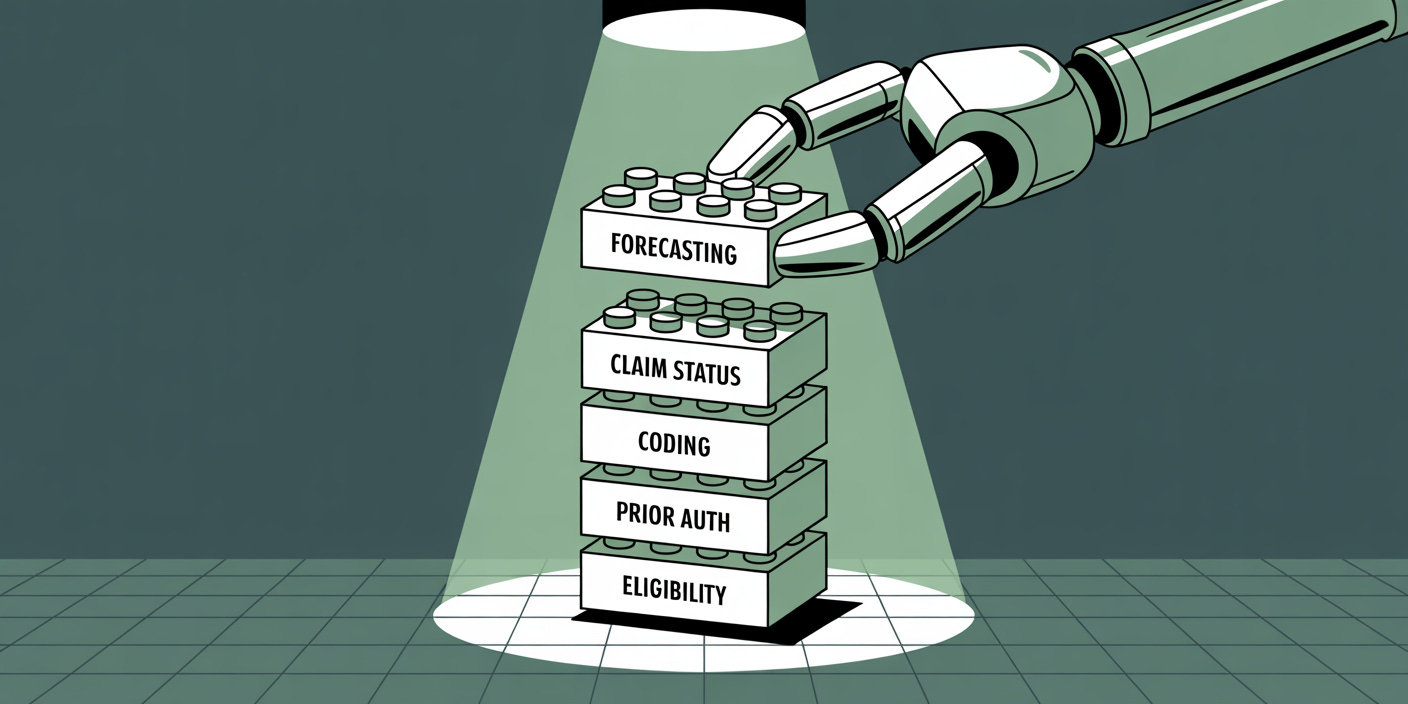
We take a different approach. Instead of building one-off flows, we build modular components — the Lego bricks of RCM. One AI agent handles a phone call. Another scrapes a portal. A third interprets an EOB. What matters is how they interface, so we can flex across edges without rebuilding from scratch.
You still need orchestration. But modularity lets us move smarter and faster. When a new exception pops up, we solve it by rearranging existing parts.
One case we didn’t expect: a regional payer’s physician roster wasn’t syncing between credentialing and billing. They kept flagging credentialed providers as uncredentialed. We automated the manual steps clinics had to take to fix it — pulling reports, placing calls, drafting emails — so things could keep moving without a human in the loop.
Q5: AI in healthcare is often inflationary — faster claims, same waste. Is Camber shifting cost curves, or just greasing the rails?
We’re not in the business of saying what care is necessary. But clinical judgment can’t work if the pipes are dirty. Our job is to clean up the inputs, so downstream decisions aren’t made blind.
A lot of waste today comes from sloppy submissions: duplicate claims, overused authorizations, concurrent claims that shouldn’t overlap. We filter that out by default. If a required field is missing, or a claim is a duplicate, we don’t submit.
The right providers should get paid. The wrong ones shouldn’t. And that starts by making sure what enters the system is accurate.
Yes, we move faster. But we also move cleaner. That’s not greasing the rails — it’s raising the floor.
Q6: What’s something that’s been unexpectedly hard in building Camber — and what do you wish more founders learned earlier?
The theme for me is focus x timing. It’s not about what to build, but when.
Healthcare is a three-stakeholder system — payers, providers, and patients — there’s infinite surface area. Once you help a provider make payroll, they start asking you to fix everything else. Not because they’re unreasonable, but because they finally trust you. If you solved this, what else can you help with?
That creates real pressure to expand too early. In behavioral health alone, you could end up building session notes, HR, payroll, accounting — and maybe one day you should. But the hard part is knowing when to say yes, and when to wait.
Great infra companies don’t just chase ARR. They apply judgment. They focus on the right things at the right time — and constantly pressure-test their direction as they grow.
In-Network Take:
Most RCM startups chase scale by selling into large groups. It makes sense on paper, but rarely lands, implements, and retains in practice.
Camber is playing a different game. It’s not automation for its own sake. It’s sequencing — like the scribes, but with faster, more visible ROI.
Help a clinic make payroll, and you don’t just win a customer. You earn the right to touch everything else. Most platforms want that kind of trust. Few are willing to earn it piece by piece.
If Camber’s right, they’ll become the financial operating layer for clinics no one else bothered to build for.
And that’s the edge: they know when to say no — to misaligned customers, premature expansions, or features that dilute the wedge. That kind of discipline is what makes infrastructure stick.
RCM isn’t sexy. But trust is. And Camber is building both, one block at a time.
💭 If this sparked something — share it with a founder, an operator, or anyone rethinking how we fund care.
Liked this one? You might also like The Ambient Scribe Stack — a breakdown on how companies like Abridge, Ambience, and DAX are going beyond the note to rewire clinical workflows. Or What WiSER Gets Right About Medicare Reform, our take on CMMI’s new innovation model putting practicality first.
In-Network is where I write about the business of care: models, margins, and the infrastructure behind how we deliver it.
→ Subscribe for sharp, honest analysis on what’s actually changing in healthcare.